Self-amplifying RNA (saRNA) is emerging as the next wave in mRNA-based therapeutics, building on the achievements of first-generation mRNA vaccines and treatments. The early platforms demonstrated that nucleic acid technologies can be scaled, regulated, and deployed rapidly; however, they also revealed real constraints in dose requirements, manufacturing costs, and equitable access. saRNA aims to address many of these bottlenecks by achieving strong and durable responses with much smaller amounts of RNA, without changing the central idea of using a temporary genetic message to encode a therapeutic protein.
For biopharma teams planning the next decade of RNA innovation, saRNA is better viewed as an evolution rather than a completely new modality. It uses the same core principles as mRNA-based therapeutics but introduces an efficient amplification step inside the target cell.
Understanding self-amplifying RNA
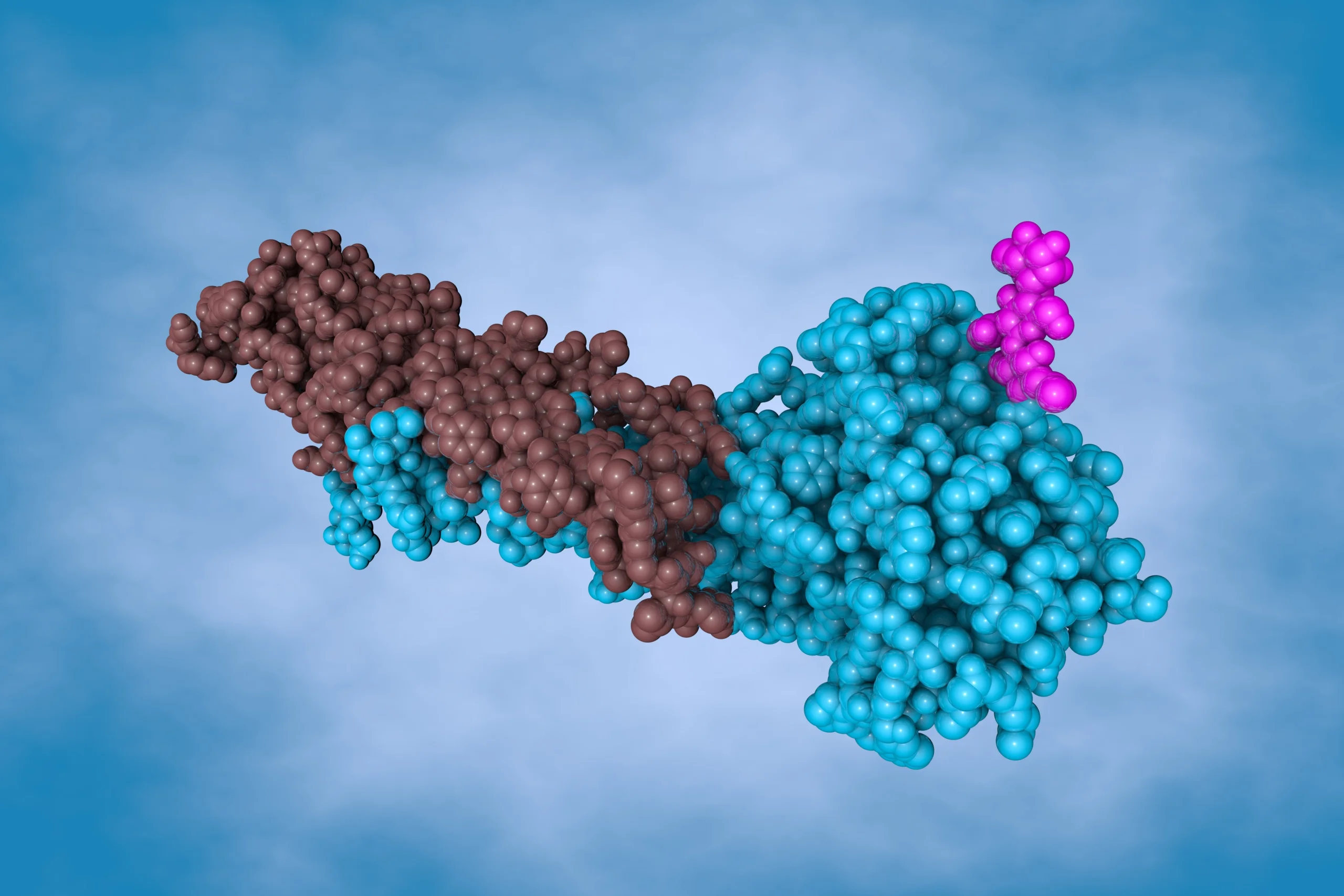
At its core, saRNA is an engineered RNA molecule that carries two key regions. One region encodes the therapeutic protein or antigen of interest, exactly as conventional mRNA does. The other region encodes viral replicase proteins that can copy the RNA once it has entered the cell.
Most saRNA constructs are derived from positive-sense single-stranded alphaviruses. In these designs, the viral structural genes are removed and replaced with the chosen therapeutic sequence, so that the RNA can replicate but cannot form infectious viral particles. After delivery into cells, the replicase proteins are translated first. These proteins then start copying the saRNA template, creating many more RNA copies than were originally delivered. The increased number of RNA templates results in higher and more sustained protein expression.
Because of this built-in amplification, saRNA can often achieve similar or stronger responses at doses that are an order of magnitude lower than conventional mRNA. That dose sparing effect makes the platform particularly attractive where manufacturing capacity, cost per dose, or global access are limiting factors.
saRNA vs mRNA: How the platforms compare
The saRNA vs mRNA discussion is not about a complete replacement of one platform by the other. It is about choosing the most appropriate technology for each scientific and commercial objective.
Conventional mRNA constructs are shorter, simpler, and easier to manufacture. They are usually well-suited for applications where higher doses are acceptable, where cold chain infrastructure is available, and where very rapid design changes are important. saRNA molecules are longer because they include the replicase open reading frame, and they may be more sensitive to shear and degradation during processing. In return, they provide amplified intracellular expression and can reduce total RNA requirements several-fold without loss of activity.
From a regulatory perspective, both platforms are based on non-integrating RNA that does not enter the host genome. However, the presence of viral replicase sequences means that saRNA requires careful evaluation of innate immune activation, persistence, and biodistribution. As more clinical data accumulate for saRNA therapeutics, confidence in the platform is growing, and review frameworks are becoming more familiar.
A practical strategy is to use saRNA in settings where dose and durability matter most, such as pandemic preparedness, resource-constrained geographies, and chronic protein expression. Conventional mRNA can be retained where construct simplicity, small size, or ultra-rapid iteration are the priority.
Lipid-based mRNA therapeutics as a delivery backbone
saRNA, like all RNA platforms, depends critically on a compatible delivery system. Lipid-based mRNA therapeutics, particularly lipid nanoparticle formulations, have become the main delivery backbone for both conventional mRNA and saRNA therapeutics.
For saRNA, the delivery design needs a few extra considerations. The longer RNA chain is more fragile, so formulation conditions must be optimised to minimise mechanical stress and chemical degradation. At the same time, the lower RNA dose per injection can reduce the total amount of lipid excipients administered, which may benefit local tolerability and systemic safety.
Developers are evaluating tissue-targeted lipids, biodegradable ionisable lipids, and alternative routes of administration, all within the broader category of lipid-based mRNA therapeutics that regulators already understand. In many cases, the same lipid nanoparticle platforms can support both mRNA-based therapeutics and self-amplifying RNA with limited adaptation, which simplifies technology transfer and scale-up.
From pDNA manufacturing to saRNA therapeutics at scale
For most RNA modalities, production starts one step earlier than RNA itself. High-quality plasmid DNA provides the template for in vitro transcription, where enzymatic reactions generate either conventional mRNA or saRNA. Robust pDNA manufacturing is therefore a foundation for any large-scale saRNA program.
Vector design, selection systems, fermentation strategies, and downstream purification at the pDNA stage all influence the efficiency and impurity profile of the final transcription reaction. Once transcription is completed, additional steps such as capping, enzymatic cleanup, and chromatography bring the RNA to the required purity and quality attributes. Many of these unit operations are already established for mRNA-based therapeutics and can be adapted for saRNA with particular attention to RNA integrity and residual DNA removal.
An integrated view of pDNA manufacturing, RNA synthesis, and formulation helps align capacity planning, raw material supply, and analytical control. Programs that combine strong pDNA manufacturing with well-designed in vitro transcription and robust formulation are better positioned to move from proof of concept to first-in-human studies for saRNA therapeutics.

Expanding the scope of saRNA therapeutics
The first clinical applications of saRNA have focused mainly on vaccines for infectious diseases, where dose sparing, rapid redesign, and scalable manufacturing provide clear advantages. However, the same features are relevant for a much wider range of indications.
In oncology, saRNA can be used to encode tumor-associated antigens, cytokines, or immune modulators, designed to trigger strong cellular immune responses at modest doses. In metabolic and rare diseases, saRNA therapeutics may offer a way to achieve longer-lasting expression of therapeutic proteins without genomic integration. There is also interest in combining saRNA with gene editing tools or with more traditional oligonucleotide development capabilities, where one modality delivers editing machinery while another fine-tunes endogenous expression.
As genomic and translational data deepen, saRNA can support more precise patient stratification, with specific payloads and dosing strategies guided by biomarkers.
Integrating saRNA into the RNA pipeline strategy
For organizations already working with pDNA and mRNA-based therapeutics, saRNA is a logical extension rather than a separate technology silo. It touches the same major disciplines, including molecular design, analytics, formulation development, clinical pharmacology, and regulatory strategy.
In practice, planning for saRNA means focusing on a few priorities:
- Building modular pDNA and RNA processes that can handle longer templates without loss of integrity.
- Extending analytical methods to characterise replicase regions, double-stranded RNA impurities, and innate immune activation markers.
- Aligning discovery, nonclinical, and clinical teams on where saRNA offers a clear advantage over conventional mRNA in terms of dose, durability, and access.
As these elements come together, saRNA can move from a specialized platform to a standard option within the broader family of mRNA-based therapeutics, especially for programs where lower doses and longer expression profiles translate directly into better patient and health system outcomes.