Overview
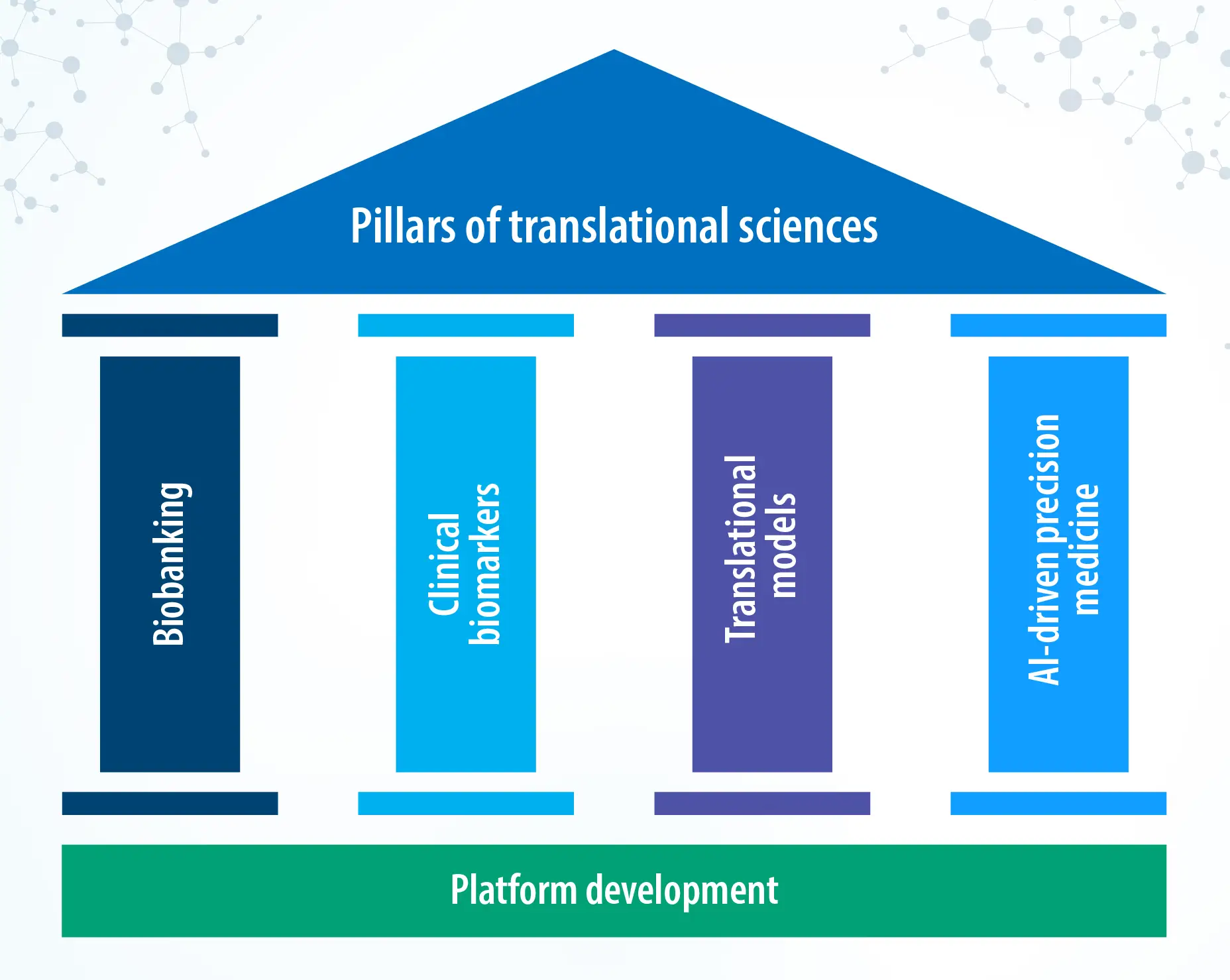
Translational research connects discovery biology to clinical reality, so promising ideas reach patients faster and safer. At Syngene, a strong base in translational sciences supports drug discovery and development, from biobanking and biomarker validation to advanced organoid and PDX models. Integrated data flows and AI help interpret ‘omics’ results and guide decisions across programs, moving the field toward the future of personalized medicine. Our translational and clinical research teams link preclinical insight with trial execution, improving the odds of success while maintaining scientific rigor and compliance.
Introduction
In the current scenario, bringing a new drug to the market typically takes over a decade and costs around $2.6 billion. Translational sciences aim to reduce both cost and time without compromising scientific rigor by dismantling silos style of working, more collaborative frameworks, and data-driven decisions from the early stages. This multidisciplinary field fosters integration across research, clinical, and regulatory domains, thereby improving success rates in clinical trials. In addition, translational research is driving a paradigm shift from “one-size-fits-all” medicine towards precision medicine, where treatments are tailored to individual patient profiles.
Biobanking
Access to high-quality, well-annotated biological samples ensures consistency, regulatory compliance, and generates reliable data for drug discovery and validation; hence, establishing a biobank is crucial for building a robust translational platform. By integrating biobanking into translational studies, we move closer to a future where a new drug is available to patients faster and is more likely to succeed. In the era of precision medicine, having a well-annotated biobank will provide a real-world context, allowing researchers to validate hypotheses and stratify patients for targeted therapies.
Syngene ‘s translational and clinical research (T&CR) department is uniquely positioned to advance translational sciences in India and develop meaningful collaborations. With an established partnership spanning >100 hospitals and clinics nationwide, we have access to rich and diverse clinical samples. These include retrospective and prospective collections ranging from fresh biopsies, FFPE blocks, snap frozen samples, blood/plasma/serum samples across multiple cancer indications, and other disease areas. All samples, whether from biobanks or directly from clinical sites, are procured in full compliance with ethical and regulatory standards, including informed donor consent and approvals from the institutional ethical committee, ensuring that our research is scientifically robust and is ethically and legally compliant.
Biomarker discovery and validation
Biomarkers are the decision-making tools in the journey of drug development. Biomarkers can be used for diagnosing a patient at an early stage, determining prognosis, pharmacodynamic response, drug monitoring, safety assessment, and predicting a particular therapy response. Identifying molecular signatures associated with disease progression and drug response, establishing reliable assays to validate biomarkers consistently across different clinical cohorts, and correlating biomarker data with real-world patient populations are the key factors to integrate biomarker studies in drug development and clinical trials.
In the era of precision medicine, clinical trials are increasingly being driven by biomarkers rather than histology-driven population selection. This allows for selecting or enriching the right cohort who is most likely to benefit from a particular therapy, which is generally referred to as “patient stratification”. Cancers like breast and lung cancer (NSCLC) have well-characterized biomarkers already known to prove beneficial for targeted therapies and personalized trial designs. However, there are cancers with limited biomarker information available, like cervical cancer, brain tumors (GBM), and bladder cancer, to name a few. For these kinds of cancers, there is a critical need to discover novel biomarkers that can significantly transform how these diseases are diagnosed, monitored, and treated.
Syngene plays a pivotal role in addressing the biomarker gaps in under-characterized cancers through its comprehensive translational research capabilities. With ready access to diverse clinical samples, robust platforms for biomarker validation, and support from Syngene’s bioinformatics team, we prove to be a strategic partner for the identification and validation of novel biomarkers.
Overall, biomarkers play a central role in translational sciences by accelerating the translation of lab discoveries into clinical practice, improving the success rate of clinical trials, and enabling tailor-made therapies for specific patient populations.
Translational models
Recent advances in translational sciences have led to the development of sophisticated in vitro models that closely resemble human physiology. Technologies such as organ-on-a-chip and 3D bioprinting represent a significant evolution over traditional 2D models. These platforms replicate the intricacy and dynamic interactions found in human tissues, thus proving to be robust models to study a drug’s efficacy and safety. Organ-on-a-chip refers to a microdevice that mimics the structure and function of human organs like the heart, lungs, and liver on the same chip. These chips are built using microfluidic technology, allowing researchers to simulate the physiological environment present in human organs, thereby enhancing the efficacy and precision of drug testing. Similarly, 3D bioprinting is an advanced tissue engineering technology that uses layer-by-layer printing of living cells with the help of bioinks and compatible biomaterials to resemble the architecture and functionality of the native tissues. These advanced models can reliably measure the efficacy and safety of a novel drug in development.
In the rapidly evolving field of translational research, the emergence of advanced animal models such as humanized mice and patient-derived xenografts has significantly enhanced drug discovery efforts. Humanized mice are genetically modified to express human genes or carry human cells, thus making them an invaluable tool to study human diseases. Humanized mice models are extensively used in oncology to test novel cancer therapies. Patient-derived xenografts are derived by implanting fragments of human tumors in immunodeficient mice. Xenograft tumors that are grown in these conditions maintain the cellular heterogeneity and microenvironment of a primary human tumor.
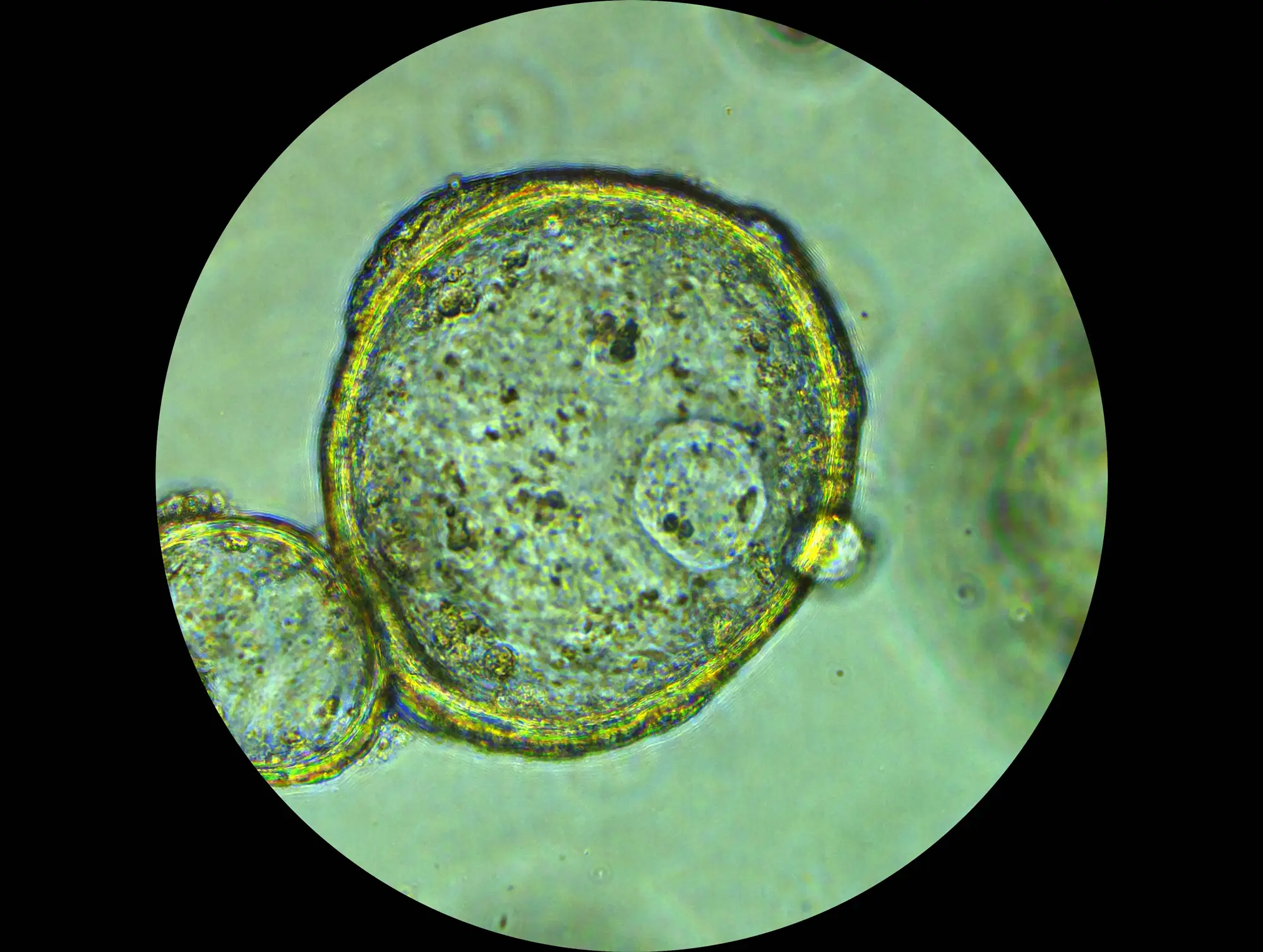
Tumor organoids are an emerging 3D in vitro model that retains the patient information and captures the biological complexity and relevance. They are cost-effective in comparison to animal models and are suitable for high-throughput drug screening. Tumor organoids are superior to traditional 2D cell culture models since they better replicate the complex cellular interactions and tumor microenvironment. Moreover, tumor organoids are strongly aligned with the FDA Modernization Act 2.0, which supports the use of non-animal models for drug discovery and development.
Collectively, these models are transforming the landscape of drug discovery and development. Since these models closely mimic the biological complexity, they help to generate critical data and provide valuable insights to reduce the formidable gap from research to clinics.
Data integration using AI tools
The integration of artificial intelligence (AI) and machine learning (ML) into the domain of drug discovery and development is a historical milestone. AI-driven analysis pipelines are adept at making accurate predictions from large datasets, a capability that is particularly useful in the “omics” world. With the application of these technologies, researchers can accelerate the identification of lead molecules, optimize formulation, and predict adverse effects more efficiently than traditional models. The potential of artificial intelligence can be harnessed to analyse a vast amount of data from scientific literature and clinical trials and identify patterns or useful biomarkers that could determine the success of a novel drug.
The potential of AI-ML is also evident in integrating the data across different phases of drug development. From initial drug design to discovery to clinical studies, AI can provide constant insight, enhancing data-driven decision-making at each step. This holistic approach maximizes the chances of developing a robust and successful drug development pipeline.
Challenges and future directions
Despite significant advancements in translational sciences, several gaps persist that can hinder the seamless translation of research findings to clinical applications. Even the advanced models like tumor organoids, organ-on-a-chip, do not fully replicate the human complexity due to the lack of other components like the immune system and stromal cells. Another challenge is the scalability of these models. While they offer remarkable results at a small scale, optimization of these assays at a larger scale and ensuring consistency and reproducibility poses a significant technical and financial challenge. Similarly, innovative in vivo animal models are revolutionizing the drug development field; however, they face significant setbacks from ethical concerns regarding animal usage and inherent biological differences between animals and humans. These gaps can lead to discrepancies in drug efficacy and safety profiling when transitioning from laboratory findings to clinical trials.
These challenges can be overcome by following a multidimensional approach that involves a) Strengthened interdisciplinary collaboration among researchers, clinicians and regulatory bodies; b) Expanding the utilization of AI-ML from the early stages of drug discovery and validation; c) Increased focus on precision medicine and novel biomarker identification and d) constant evolution of translational models like multiorgan chip along with CRISPR based gene editing tools or co-culture of immune system with tumor organoids to recreate the natural conditions found in human body.
Syngene’s edge in translational research
Syngene offers a comprehensive workflow from preclinical discovery to clinical development that improves data continuity, accelerating the development of novel therapies and reducing the time required to bring innovative drugs to market. In addition, our state-of-the-art facilities, along with excellent scientific skillset, ensure data quality and scientific rigor.
Traditionally, CROs focus on either drug discovery or clinical studies; Syngene, on the other hand, acts as a scientific collaborator offering a seamless integration of both. This unique blend empowers our clients to make faster, more informed decisions. Syngene’s multidisciplinary model works well for diverse therapeutic areas, notably oncology, rare diseases, and inflammation. Syngene has supported submissions to the FDA, EMA, and other global agencies, making it a reliable partner for IND-enabling studies, clinical trial documentation, and regulatory compliance. Syngene’s strategic location provides access to diverse patient populations, enabling rapid recruitment for clinical trials. Combined with cost-effective strategies, we are offering high-quality, timely delivery of our studies.
To stay ahead of industry needs, Syngene is actively investing in next-gen technologies like organoid models, clinical biomarker studies, and AI-powered data-driven analytics to help our collaborators remain at the forefront of scientific excellence and clinical advancement.
Conclusion
As diseases evolve and new health conditions emerge, the need for rapid and reliable translation of research into clinics becomes increasingly critical. Translational sciences play a pivotal role in driving innovation and enabling data-driven decisions that expedite the safe and effective implementation of research findings into clinics. Moreover, it supports the advancement of personalized medicine that tailors treatments based on genetic and molecular profiling of individual patients, thereby reducing the risk of adverse effects. Collectively, translational sciences not only help in faster delivery of a drug to the market but also enhance the precision and effectiveness of a treatment, ultimately improving patients’ quality of life.
Syngene has an experienced and dedicated team, including state-of-the-art facilities at the Translational and Clinical Research (T&CR) department. Over the years, we have successfully delivered numerous projects to our national as well as international partners. Our comprehensive end-to-end workflow spanning preclinical studies, translational models, bioanalytical services, early and late phase clinical trials, along with regulatory support, ensures the generation of high-quality data across diverse disease areas. This makes Syngene a reliable partner for translational services to accelerate drug discovery.